Proteins that outwit emerging and re-emerging viruses
Article by: Emily Caldwell
Originally Published
A family of proteins best known for their role in diminishing HIV infectivity may have the goods to outwit other emerging and re-emerging viruses, scientists have found.
The key to their newly discovered power: enhancing the signals sent within immune cells to unleash one of the most potent fighters in the innate antiviral response, proteins called type I interferons.
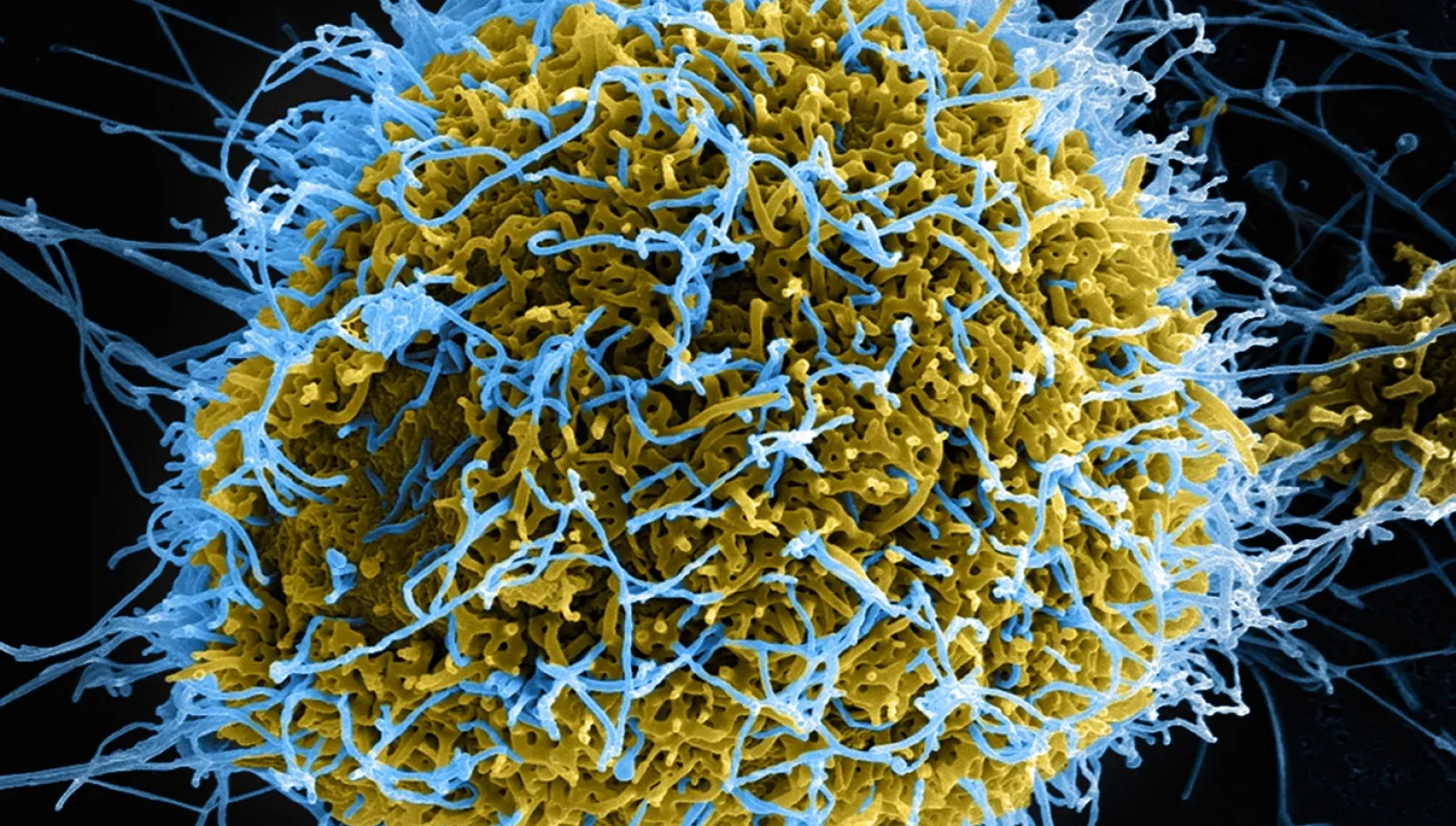
Experiments in cell cultures showed that the cell-signaling activities of these proteins, from the SERINC family, helped protect cells from infection by HIV, Ebola and Zika viruses. The researchers are currently testing whether this function is also effective against SARS-CoV-2, the virus that causes COVID-19.

It’s one thing for a protein to act directly against a specific virus, as SERINC5 has been shown to do by incorporating itself into the HIV particle during viral production. But it’s another thing entirely to reveal that a protein has an enhancing effect on an essential antiviral cell signaling pathway upon infection of host cells, said senior study author Shan-Lu Liu, professor of virology in the Department of Veterinary Biosciences at The Ohio State University.
“Viruses can get around direct antiviral effects,” said Liu, also an investigator and associate director in Ohio State’s Center for Retrovirus Research. “But if this protein can also modulate key pathways without acting directly on the virus, then a virus may have limited capacity to counteract it.
“If this family of molecules can do this in animals and humans, then you may think about whether it could be used in a broad antiviral therapy.”
The research is published today (Sept. 14, 2021) in the journal Science Signaling.
Liu has studied what he calls the “evolutionary arms race” between HIV and the human immune system for years and led a 2019 study that described how an HIV protein called Nef can get the upper hand in that fight – specifically by interfering with SERINC proteins in virus-producing cells.
In this study, Liu and colleagues took a closer look at SERINC5’s functions in target cells during the next viral infection stage. They found that in addition to boosting the signals that produce type I interferons, SERINC5 has the same effect on signals that generate another component of the early antiviral response – NF-kB inflammatory cytokines.
SERINC5 doesn’t modulate this signaling system on its own – it joins forces with other proteins called MAVS and TRAF6. But some of its exact behaviors are still a mystery, Liu said.
In cell cultures in which viral infection had been initiated, the researchers observed that SERINC5 relocates itself from the cell surface to just outside the membrane around the mitochondria, a cell’s power center – an unusual move. Once there, SERINC5 teamed up with MAVS and TRAF6 to form a big, multifaceted complex – a likely explanation for why its role is so influential on what happens next in the signaling pathway.
“The aggregation of these proteins means they need each other – and this is an exciting finding,” said Liu, also co-director of the Viruses and Emerging Pathogens program in Ohio State’s Infectious Diseases Institute. “A big complex like this can recruit additional molecules, enhancing the efficiency of the signal transduction pathway.”
These recruited molecules are part of a cascade of messages that lead to type I interferon production and NF-kB inflammatory cytokines from virus-infected cells, both of which play a crucial role in limiting viral infection in the early stage. In experiments utilizing multiple types of human and animal cell cultures, this mechanism was seen to inhibit infection of cells by HIV, Ebola and Zika viruses.
In contrast, when cells were modified so they didn’t produce the SERINC5 protein, these viruses took over cells and replicated more – suggesting how important SERINC’s role is in the process that potentiates the primary antiviral response of host cells.
This work was conducted in two members of the SERINC family, SERINC3 and SERINC5, but Liu speculated that other versions may have similar effects. But there is still a lot to learn – such as what triggers SERINC5 to relocate itself from the cell surface to mitochondria, and what its normal cellular functions are when there is no virus around.
As for whether the protein’s functions can suppress the COVID-19 virus, Liu is optimistic.
“My speculation is the SERINC protein would have an effect because we know type I interferons are so important to controlling a virus in the early stage, and this molecule can enhance the type I interferon response,” he said. “Finding one protein that can modulate a key pathway that has a broad antiviral effect – well, you can imagine this protein has a broad antiviral function.”
This work was supported by the National Institutes of Health and the National Cancer Institute (NCI).
Co-authors include Cong Zeng, Tianliang Li, Jingyou Yu, Yi-Min Zheng, Jacob Yount and Haitao Wen, all of Ohio State, and Abdul Waheed and Eric Freed of the NCI HIV Dynamics and Replication Program.